Our Blog
Our latest blog post of physiotherapy
and massage.
Forefoot vs rearfoot striking
By Matt Bushell The publishing of the book ‘Born to run’ by Christopher McDougall propelled the barefoot movement and minimalist shoes into the popular running world around 2009. And while the subject tends not to be as all-consuming as it once was, it’s left behind a question that we hear regularly from both experienced and aspiring runners; ‘should I run with a forefoot or rearfoot strike?’. Foot strike can be broken into 3 main categories; rearfoot, where your heel contacts the ground first, midfoot, where you contact the ground with a near flat foot and finally forefoot, where the ball of the foot touches the ground with the heel noticeably raised. Foot strike is variable in all runners and in general, running slowly will lend itself to more of a heel/midfoot strike. As pace increases, we move through to forefoot striking during sprinting. Similarly, hills often demand heel striking on descents and forefoot striking on climbs. When it comes to running, neither of these styles is categorically correct or incorrect. As with any movement in the human body, changes in pattern equal changes in demand on different structures. Each of these running styles is achievable for most people, but they require your body to deal with different forces so if you’re thinking of changing your running style, it’s best to prepare your body for the changes (generally through a strength and conditioning program) before you try and do too much volume (distance) with your new running style. Rearfoot strike Rearfoot striking is by and large the most common running style you’ll observe in the casual or weekend warrior running groups. It typically involves a longer stride length, a slower turn-over of your legs (less steps for an equivalent pace) and some cushy shoes to protect your heels (Ahn et al. 2014). The greatest detractor of the rearfoot striking style from an efficiency perspective is the fact that your foot contacts the ground a long way in front of your centre of mass which creates a braking force (Lierberman et al. 2015). Each time your heel strikes in front of your centre of mass, you lose some of your forward momentum and you need to expend more energy on your next push off to maintain your pace. In terms of forces, rear root striking increases the load on the hip and knee. Your quadriceps, hamstrings and your tibialis anterior (the small muscle on the front of your shin) then have to deal with increased work loads. Forefoot strike For the purposes of this article, we’ll combine both midfoot and forefoot striking effects below. Generally speaking, they’ll have similar effects in terms of structures loaded with load increased in the forefoot striking compared to midfoot. Forefoot striking generally requires an increase in cadence (footsteps per minute) for the same velocity as rearfoot striking. This increase shortens your stride length slightly and brings your ground contact point back underneath your body. This has the positive effect of reducing the braking forces mentioned earlier (Lieberman et al. 2015). Landing with a mid or forefoot strike increases the load on the ankle and foot complex and asks more of your calf and achilles tendon (Ahn et al. 2014, Almonroeder et al. 2013). It will also normally reduce your vertical impact loading rate. This means the impact force of your foot hitting the ground is spread over a greater time thereby reducing the magnitude of load your body has to deal with at any one time. Injury Rates During the peak popularity of the barefoot/forefoot striking movement, there was a thought that it may reduce injury rates. After studying runners over longer periods of time, we now know injury rates are similar regardless of which style of foot strike you employ (Zhou & Ugbolue 2019). Where we do see a possible increase in injury rates is when people attempt to change their running style. This is likely due to increased demand on the body in a way that it is not accustomed to. Running style is individual and large or sudden changes tend to have a negative impact on our body. However, sometimes changing your running style slightly can help to improve speed, increase endurance or overcome niggly injuries. If you’re looking to make a change in running style, or have an injury you’d like to address, your physio can help to provide a considered approach to your running frequency, volume, intensity and provide you with a complimentary strength program to ensure your body is up to the new challenges. Ahn, A., Brayton, C., Bhatia, T., & Martin, P. (2014). Muscle activity and kinematics of forefoot and rearfoot strike runners. Journal of Sport and Health Science 3 (2), pg 102-112. Almonroeder, T., Willson, J. D., & Kernozek, T. W. (2013). The effect of foot strike pattern on achilles tendon load during running. Annals of Biomedical Engineering 41, 1758-1766. Lieberman, D. E., Warrener, A. G., Wang, J., & Castillo, E. R. (2015). Effects of stride frequency and foot position at landing on braking force, hip torque, impact peak force and the metabolic cost of running in humans. Journal of Experimental Biology 218 (21), 3406-3414. Zhou, H., & Ugbolue, U. C. (2019). Is There a Relationship Between Strike Pattern and Injury During Running: A Review. Physical Activity and Health, 3(1), 127–134.
Flexibility – To Stretch or Foam Roll?
Matt Bushell Flexibility is the ability for a joint (or a combination of joints) to move through an unrestricted and pain free range of motion. The amount of movement available is affected by many structures including joint shape, joint capsules, ligaments, muscles, tendons and nerves. Increasing our flexibility can give us many advantages including increased movement options, force generation/dispersion and improving completion of functional tasks. Often it is assumed that an increase in range of motion at a joint after stretching is due to a muscle being lengthened. Interestingly, it may actually be due to an increase in your tolerance to tension which then allows you to stretch your muscle further and allow greater movement through the joint (Page. P, 2012). Once you reach the maximum amount of tension your brain and nervous system deems safe, your muscle will reflexively tighten to stop any further stretch – much like a safety switch. Therefore those who are ‘more flexible’ may simply have a greater natural tolerance to tension which allows them to bend their joints further than others. After stretching, the increased tolerance to tension only lasts for a period of time and then we tend to return to our individual baseline. The question is, will static stretching or foam rolling give you the best increase tolerance to tension and therefore flexibility? Static Stretching Static stretching involves stretching a muscle to a point (often near your maximum) and maintaining that stretch for an extended period. In theory, holding the stretch increases the tolerance of muscle spindle cells (stretch receptors in the muscle) to the tension applied and allows them to deal with greater tension for a time post-stretching. Research has found there is generally no further improvements in range of motion after 2-4 sets of 15-30 second holds and results last from less than 1 hour to a couple of days. (Knudson, 2010) Foam Rolling If you’ve never seen one, a foam roller is a self-massage tool used to ‘roll out’ your muscles or sore spots often referred to as trigger points. Theoretically the pressure from the roller stimulates pressure receptors in our skin and causes the brain and nervous system to reduce muscular activity. This then allows greater tension before activating the safety switch and tightening up the stretched muscle. Foam rollers can come in different sizes, densities and can vary in surface texture from smooth to bumpy or spikey. Rolling for 2-5 sets of 30-60 seconds has been found to have a positive effect on our flexibility with effects lasting for between 10 minutes and 7 days (depending on the individual). Bear in mind, from a Physiotherapists’ perspective the purpose of foam rolling is not purely to increase range of motion (and therefore flexibility), but also to reduce intramuscular tension (muscular knots) to facilitate a more supple and functional muscle. How about a combination? Combining both static stretching and foam rolling seems to provide a significant increase in range of motion over either modality in isolation. However, the duration of this larger increase appears to last for approximately 10-60 minutes (Mohr, 2014). This suggests it’s most useful application is right before a sporting event or exercise program that requires you to have increased flexibility for a time. It is important to mention though that static stretching may have a negative effect on power and strength output, so if your sport or exercise program requires high levels of strength or power, limiting yourself to foam rolling beforehand may be the most sensible option. Along with other techniques to address muscle length, physiotherapists can also use manual therapy and exercises aimed at joints, joint capsules, ligaments and tendons to positively influence your flexibility. As mentioned above, stretching and rolling results can vary quite a bit from one individual to another, so we recommend seeing your physio if you’d like an individualised flexibility plan. Knudson, D. (2010). The biomechanics of stretching. Journal of Exercise Science and Physiotherapy 2, 3-12. Mohr, A., Long, B., & Goad, C. (2014). Effect of Foam Rolling and Static Stretching on Passive Hip-Flexion Range of Motion. Journal Of Sport Rehabilitation, 23(4), 296-299 Page, P. (2012). Current concepts in muscle stretching for exercise and rehabilitation. International Journal of Sports Physical Therapy 7 (1), pg. 109-119.
Creams, Gels & Lotions
There are so many good (and some not so good) pain relief and natural anti-inflammatory topical creams on the market at the moment, it can be a bit confusing as to what is right for you. Here at Queen Street Physiotherapy we stock a small range of different natural creams to cover all of your needs and preferences. Antiflamme: An old favourite of everyone who uses it. With a carefully selected range of naturally-derived plant based oils including Arnica, Hypericum, Calendula and Peppermint. It helps to relieve minor joint and muscle pain, reduce mild muscle inflammation, and assist in the management of muscle strains and sprains. It has a thick cream consistency and a pleasant minty smell. It is a wonderful alternative to the pharmaceutical anti-inflammatory creams for those who are looking for a plant based alternative. Bullet & Bone Muscle Activating Rub: This warming cream is another that can be used to alleviate muscle aches and pains. As it is lightweight and rapidly absorbed, it is designed to be used before exercise to accelerate warm-up and reduce the risk of injury. This lotion contains willow bark, meadowsweet and clary extract which offer natural anti-inflammatory effects. Better Nature Pain Relief Cream: This is another new one to our shelves which has been created from naturally sourced plant ingredients including Eucalyptus, Arnica, Hypericum, Rosemary and Wintergreen. It has a very natural fragrance to it so if you prefer something with less smell but with the same natural anti-inflammatory properties then this may be the cream for you. Please feel free to ask about any of these creams when you are next in the clinic. The Physiotherpist’s are happy to include them in your treatment so you can try before you commit to buying. Whilst these products are not medicated, if you are unsure about what is safe to use on any specific skin conditions or if you are pregnant please consult with your doctor or pharmacist.
Hamstring Strains
Acute hamstring strains are common injuries for many popular sports, including various football codes, hockey, cricket and track and field. Hamstring injuries are the most common injury in Australian rules football, constituting 15% of all injuries, with an incidence rate of 6 injuries per approximately 40 players per season, and a prevalence rate of 21 missed matches per club per season. Similarly, in the English Premier League, hamstring strains make up 12% of all injuries. Acute hamstring strains also have the highest recurrence rate of any injury, a rate of 34% in Australian rules football and 12% in the English Premier League (Brukner & Khan 2015). There are two types of hamstring strains: Type I and Type II Type I Acute Hamstring Strains: Type I hamstrings strains are the more common injury type, which often occur during high speed running. They usually involve the long head of biceps femoris, most commonly at the proximal (upper) muscle-tendon junction. These generally cause a more marked acute decline in function but typically require a shorter rehabilitation period than Type II injuries. Case studies suggest that hamstrings appear to be the most vulnerable during the end of the swing phase of sprinting, where they are highly activated as they work eccentrically to decelerate the swinging tibia (shin) and control knee extension in preparation for foot strike. Symptoms usually consist of a sudden onset of pain in the hamstring region that interrupt the ability to run. Type II Acute Hamstring Strains: Type II hamstring strains often occur during movements leading to excessive lengthening of the hamstrings when the hip is in flexion, such as high kicking, slide tackles in soccer or performing the splits. These injuries more commonly occur in sports that require large amplitude movements such as ballet and gymnastics. The common mechanism of injury in these instances is an excessive stretch into hip flexion. These injuries are often located close to the ischial tuberosity (base of the buttocks on the pelvic bone) and can involve the semimembranosus (one of the hamstrings’) tendon. Type II strains often cause a less dramatic acute limitation than Type I strains, though their rehabilitation is often longer. Passive stretching and heavy-load exercises seem to aggravate these hamstring injuries. Signs and Symptoms: An acute hamstring strain results in a sudden, minimal to severe pain in the posterior thigh, sometimes with a characteristic “popping” or tearing impression. Swelling and bruising are possible but may not occur for several days after the date of injury. Loss of joint active range of motion in the knee and hip can be apparent as well as decreased strength and length of the injured hamstring. Rarer symptoms can include numbness, tingling, and distal extremity weakness. These symptoms require further investigation into sciatic nerve irritation as a result of either impingement of the nerve or secondary injury. Large hematomas (swollen muscular bruising) or scar tissue can be caused by complete tears and avulsion injuries. Hamstring strains are categorised in 3 groups, according to the amount of pain, weakness, and loss of motion: Grade 1 (mild): just a few fibres of the muscle are damaged or have ruptured. This rarely influences the muscle’s power and endurance. Pain and sensitivity usually happen the day after the injury. Walking is usually able and the knee can still bend normally. Grade 2 (medium): approximately half of the fibres are torn. This will influence the muscle’s power and endurance, and can include a limp with gait. There is occasional swelling, often bruising (which may or may not come to the skin surface) and pain which can be reproduced by bending the knee against resistance. Grade 3 (severe): ranging from more than half of the fibres ruptured to complete rupture of the muscle. Both the muscle belly and the tendon can suffer from this injury. It causes large swelling, bruising and pain. The function of the hamstring muscle can’t be performed anymore and the muscle shows great weakness. Prognosis of Hamstring Injuries: The following factors have been shown to be associated with increased length of time to return to play: Time to walk at normal pace pain-free has been shown to be significantly associated with return to play time (>1 day = 4x more likely to take >3 weeks). Combining this with a past history of hamstring injury within 12 months results in a 93% chance of taking longer to return to play. Days to jog pain-free is the strongest predictor of time to return to play: 1-2 days = < 2 weeks 3-5 days = > 2 weeks > 5 days = > 4 weeks The closer to the ischial tuberosity in a biceps femoris injury, the more prolonged the time to return to pre-injury level. Injury to the tendon of the semimembranosus muscle is associated with a recovery period of twice as long of those without tendon injury. The length and cross sectional area of the tear results in prolonged return to play. (Brukner & Khan 2015) Risk Factors for Acute Hamstring Strains: Risk factors for a hamstring strain may be intrinsic (patient related) or extrinsic (environment related). Body Mass Index (BMI), height and weight have been ruled out as factors for hamstring strains through the use of functional performance tests. Intrinsic factors: Age: Athletes from older age groups are at an increased risk of an acute hamstring strain. For example in Australian rules football, players older than 23 years of age are 4 times more likely to sustain an acute hamstring injury. This may be related to reduced hip flexor length, but it has also been suggested that it could be in relation to degenerative changes at the lumbosacral (base of the spine) junction. Past history: In comparison to injury-free athletes, those with a past history of hamstring injury demonstrate differences in hamstring muscle volume, scar tissue and contraction mechanics. The presence of scar tissue creates higher rates of localised tissue strains in adjacent muscle fibres. Athletes with a history of other lower limb or lower back injuries
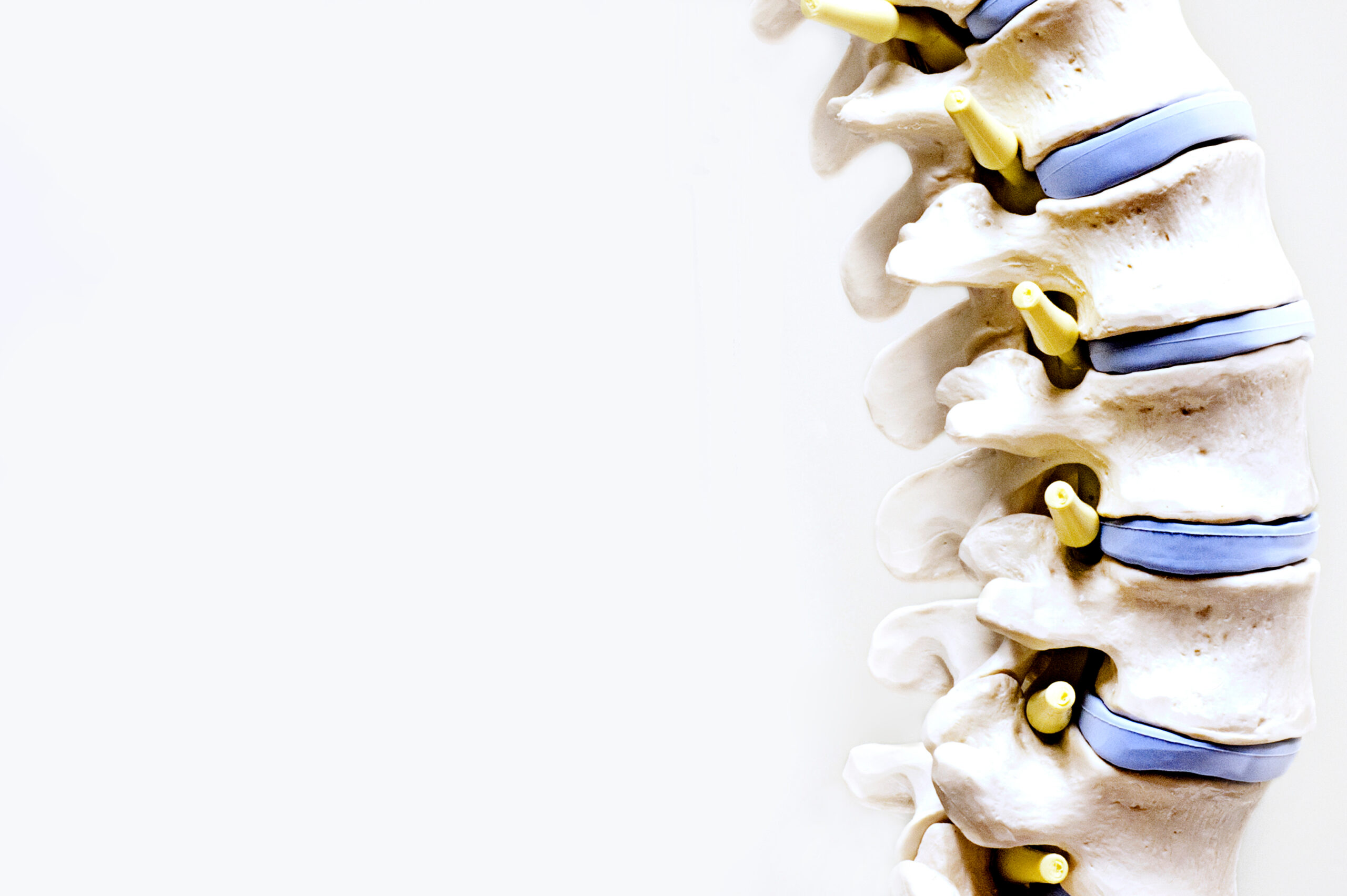
Motor Vehicle Accidents (MVA) and Physiotherapy
A car accident can not only be a traumatic experience mentally but it can result in ongoing physical injuries. Injuries could include fractures, soft tissue damage (intervertebral joints, disc, ligaments, muscle), spinal or nerve damage, traumatic brain injuries, impaired vision or impaired hearing. Over a 12 month period in 2017-18, almost 40,000 people were admitted to hospital with injuries after a road accident in Australia. In 2020, Queensland accounted for 225 fatalities (or 21% of fatalities across Australia) in car accidents, making it the third most prevalent state. Anatomy and whiplash: The spinal column is made up of vertebrae (bones) that sit on top of each other separated by discs (cartilage rings), and connected at joints which are supported with ligaments. The spinal cord runs down the middle of the vertebrae and nerves exit from this at each level of the spine. Surrounding all of this, is various groups of muscles, some with small stabilising functions and some with larger movement functions. These structures all work together to help protect your spinal cord and facilitate movement of your torso and head. Whiplash is a sudden force exerted on the neck which forces it to move rapidly and overstretch and injure these structures. Whiplash and other trauma from a car accident most commonly causes micro trauma to several of these structures (joints, ligaments, muscles) rather than just one specific area. Symptoms: Due to the shock of the accident, pain isn’t always felt immediately. It may present 24-72 hours following the incident. Even a low impact MVA can result in pain. This is most common in the neck, head and shoulders, followed by the lower back. However pain can occur anywhere throughout the body following an MVA. Depending on the individuals age, symptoms and range of movement, a doctor may or may not recommend that a scan is required. Pain may increase with various activities, like work, exercise, sleeping, sitting or participating in your hobbies. Apart from pain, individuals may also experience: Loss of movement Headaches Pins and needles or burning sensations Numbness Disturbed sleep Tiredness **Stress is also common after an accident, particularly when being in a car again. It is important to address this if present, to avoid long-term anxiety-related issues. Where able, monitor any memory loss, concentration impairment, nervousness or irritability, sleep disturbances, fatigue or feelings of depression. Treatment: Early intervention from a physiotherapist is important to address these injuries, guide your recovery process and help prevent the risk of long-term damage. With treatment, most patients recover in a few days/weeks to 3 months after the injury. The difference in recovery times is highly dependent upon the severity of the injury, the ability to access regular physiotherapy and activity of daily living requirements (work and home). It is especially important to address whiplash injury early, as symptoms still experienced by the 3 month (post-accident) mark can often become chronic. Physiotherapists promote recovery through manual & massage therapy for pain relief, education on management at home and work, and advice on appropriate exercises to encourage movement and strength around the neck and shoulders. Exercises can also be prescribed for ocular-motor control for visual disturbances following an MVA. **Besides the damages to the vehicle, being in an accident can take a financial toll in terms of covering medical expenses and time off work. Some individuals are eligible to submit an insurance claim or if the accident happened on the way to/from work, the individual may be eligible under workcover. If you are unsure, feel free to contact our reception for some advice on who may be able to assist.
Relative Energy Deficiency in Sports syndrome (RED-S) and stress fractures
Nutrition is an extremely essential component of an athlete’s lifestyle for performance purposes. Although overconsumption of food is a common issue in Australia today, it is not uncommon for athletes to under consume the recommended calorie intake for their level of activity. This can cause a serious syndrome called Relative Energy Deficiency in Sports (RED-S). RED-S is more common in female athletes but can be an issue for both male and female alike. Put simply, an athletes calorie intake requirements often sit higher than a sedentary individual due to the amount of energy they burn to train. If an athlete does not consume enough calories to meet the demands of the activity, they’re expending more energy than they’re intaking. For women, the stress placed on the body from insufficient fuel can lead to a loss of menstruation (also known as amenorrhea). This tends to evolve into detrimental effects on the hormonal pathways in the body, including decreasing oestrogen levels, which can weaken bones. The end results from an sporting perspective is increased occurrence of stress fractures, reduced energy and endurance levels as well as reduced concentration. For female athlete’s the syndrome is characterised by these three issues; disordered eating, loss of menstrual periods and decreased bone mineral density. These three interlinking problems are often referred to as the female athlete triad. It is important to note that NOT all three symptoms (poor calorie intake, amenorrhea and decreased bone mineral density) must be present to have a diagnosis of RED-S. Sometimes only two of the three components are present. Not only are stress fractures and low energy a concern when RED-S is occurring. RED-S has also been related to cardiovascular issues, lowered immunity, reduced protein synthesis and limitations on growth and development. Symptoms to watch out for: The bottom line for RED-S: Not only will the performance of the athlete be compromised with RED-S, but a multitude of serious health risks can also occur. Therefore, it is particularly important that we educate both younger athletes, and coaches of athletes, to monitor any who may present with disordered eating habits/low eating habits/low BMI. Importantly, a simple lack of education regarding dietary intake requirements may be the causative factor; this can be rectified with some guidance to provide a dietary intake solution. It should however be noted that athlete stereotypes and mental health has the potential to play a major role for athletes with RED-S. Assistance regarding the athletes psychology should be sought where education alone is unsuccessful. If left untreated this syndrome could not only end an athlete’s career through injury, but could also have serious detrimental effects to long-term health – increasing the risks of cardiovascular disease and osteoporosis, both of which decrease life expectancy in individuals. Stress Fractures: Repetitive loading of bones can lead to increased stress within the bones. This then has the potential to develop into stress fractures as a result of fatigue failure of the bone. Stress fractures account for up to 20% of all sports medicine clinic injuries under normal circumstances without additional influence from RED-S. Track and field athletes have the highest incidence of stress fractures (Brukner, Bennell & Matheson 1999). In a normal environment, musculoskeletal integrity is maintained by a balance of fatigue damage with remodelling activity, stimulated by normal repetitive low-intensity loading forces. The rate of remodelling responds to the loads through the bone, which includes the forces transferred from surrounding muscle activity. High levels of bone stress, through an increase in activity, may lead to higher rates of fatigue damage where the remodelling response may not be able to cope. This then manifests clinically as a bone stress injury. Overload can be applied to the bone through two mechanisms: There are two important risk factors to consider for bone stress injuries. The first being a rapid increase or change in the load on the bone, the second being the energy imbalance between calories expended and calories taken in. As mentioned, energy imbalance causes hormone irregularity and impaired bone health. Stress fractures can be categorised into low-risk and high-risk fractures. Low-risk fractures generally require no treatment other than rest. The sites where these fractures occur tend to be on the compressive side of the bone and respond well to activity modification. Low-risk fractures are also less likely to reoccur, become a non-union, or have any significant complication should they progress to a complete fracture. High-risk fractures are often harder to diagnose, and often tend to progress to non-union or complete fracture, may require surgical management, and may reoccur. Symptoms: Treatment: Treatment is often multidisciplinary requiring a general practitioner, a dietician and a Physiotherapist for stress fracture. In addition there is potential for a sports psychologist to be required if RED-S syndrome is the primary factor for the stress fracture. Physiotherapist provide guidance in two ways: Please seek the advice of your Physiotherapist and Dietician if you have concerns with calorie intake, program loading or pain from suspected stress fractures. Mountjoy M, Sundgot-Borgen J, Burke L, et al 2014. The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S) British Journal of Sports Medicine 2014;48:491-497. Brukner P., Khan K,. 2015. Clinical Sports Medicine, Sports concussion; 600-617
Patellofemoral Pain Syndrome (PFPS)
The knee consists of two major joints: the tibiofemoral joint – the main hinge joint of the knee, and the patellofemoral joint – which acts as a pulley mechanism to allow for the smooth transition of knee extension to flexion. To achieve this, the patella (kneecap) sits in a groove in the femur (thigh bone), which is covered in cartilage. The patella glides over this cartilage whenever the knee moves. Injury mechanics: Altered tracking of the patella during knee flexion and extension due to biomechanical changes often results in pain around the knee. This is due to a change in the directional forces applied to the patella on movement. These changes cause the patella to shift out of the groove and apply pressure to the femoral condyles (the bony prominences beside the femoral groove) and thus can cause overuse/overload (overpressure) on that part of the femur. The pressure can result in pain, discomfort or irritation and eventually contributes to damage of the cartilage surfaces. This is called Patellofemoral Pain Syndrome (PFPS). PFPS can occur as a result of trauma to the patella. However, it is more commonly associated with multiple factors including anatomical or biomechanical abnormalities and/or muscular weakness, imbalance and dysfunction. The orientation of the patella varies between individuals, it can also vary between left and right limbs in the same individual, which can result in anatomical malalignments that contribute to PFPS. A common example of this imbalance is seen between two of the quadricep muscles. In many situations the Vastus Medialis Obliquus is weak in comparison to the Vastus Lateralis. This results in the Vastus Lateralis exerting a higher force on the patellofemoral joint and causes a lateral glide, tilt or rotation of the patella. This applies pressure on the lateral aspect of the femur. Repetitive pressure to this lateral aspect then leads to overuse of the area and eventually inflammation and pain of the lateral knee joint occurs. Other Potential injury mechanics of PFPS: Tightness in the iliotibial band – which places excessive lateral force on the patella and can also externally rotate the tibia, altering the biomechanics of the patellofemoral mechanism. Tight hamstring muscles – Which applies posterior forces on the knee, causing pressure between the patella and the femur. Weakness of hip external rotators muscles – which results in compensatory foot pronation, again altering the tracking of the patella through changes in the tibia’s position in relation to the femur. Tight calf muscles – Which can lead to compensatory foot pronation (flat-footedness) and can increase the posterior force on the knee. Signs and Symptoms: In most cases, symptoms of patellofemoral pain syndrome develops gradually. Symptoms usually get worse with activity and may include: A dull, aching pain in the front of the affected knee, behind or close to the patella. Pain during activities that bend the knee, including squatting or climbing stairs (especially downstairs). Pain after sitting for extended periods of time where knees are kept bent. Crackling or popping sounds in the affected knee when standing up or climbing stairs. Pain that increases with sudden changes in regular playing surface, sports equipment or activity intensity. Prognosis: PFPS has no set time period for healing. It can become a long-term condition if left untreated as the mechanism which cause the injury do not tend to dissipate on their own; meaning the biomechanical insufficiency needs to be addressed. The longevity of the condition can often lead to greater levels of degeneration on the affected structures and eventually cause early onset arthritis or require surgical intervention. Therefore it is important to diagnose and treat this condition sooner rather than later. What can your physiotherapist do for you? Physiotherapists treat PFPS in a few ways. Firstly, they can loosen off of tight muscular structures such as the iliotibial band, hamstrings, quadriceps, hip external rotators and calf muscles through soft tissue massage, myofascial trigger point releases and superficial dry needling. This will help to alleviate painful symptoms which in turn can enable a larger range of motion for activities of daily living and strengthening exercises. Secondly, they can prescribe exercise to help address the underlying biomechanical insufficiency. No only will this help to reduce immediate symptoms, it will also help to prevent PFPS returning in the future. Prescription of exercise is of significant importance when managing PFPS. Strengthening of the quadriceps is a key factor of PFPS rehabilitation (Bolgla & Malone 2005), in particular increasing the strength of the Vastus Medialis Obliquus has a positive effect on PFPS symptoms by increasing the medial forces projected onto the patella, counteracting the lateral shift of the patella. In addition to strengthening the quadriceps, it is important to strengthen the abductors and external rotators of the hip. Nakagawa et al 2008, found that increasing the muscle strength of certain muscle groups (quadriceps, abductors and external rotators of the hip) has a positive impact on PFPS symptoms. Furthermore, it has been recommended that eccentric strength training be implemented to the hip abductors in particular to treat PFPS. Eccentric strength training is the loading of a muscle whilst it is lengthening. And lastly, in addition to strength training, Physiotherapists will also prescribe balance drills. Akseki et al 2008 & Clark et al 2000 agreed that the proprioceptive quality of PFPS patients was decreased. Proprioception is the perception or awareness of the position and movement of the body, which is a key component in the bodies ability to balance. Poor proprioceptive ability has been found to have direct correlation with other injuries such as anterior cruciate ligament injuries to the knee. Therefore it is a key factor in injury prevention for the affected knee. If you have been experiencing knee pain on movement, and are worried PFPS may be occurring, contact your Physiotherapist for some timely advice! Bolgla L & Malone T, 2005. Research Review: Exercise Prescription and Patellofemoral Pain: Evidence for Rehabilitation.Journal of Sport Rehabilitation 14(1):72-88 Nakagawa TH, Muniz TB, Baldon Rde M, Dias Maciel C, de Menezes Reiff RB, Serrão FV.
Concussion
Concussion is defined as a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces. The brain has the consistency of gelatin. It’s cushioned from everyday jolts and bumps by cerebrospinal fluid inside the skull. A violent blow to the head and neck or upper body can cause the brain to slide back and forth forcefully against the inner walls of the skull. Concussion is currently a major area of study in medical circles, particularly surrounding the wellbeing of athletes’ long term health. Concussion is particularly prevalent in contact sports as it’s mechanism of injury is often associated with transmission of forces on the head, as well as the rapid acceleration and deceleration forces on the brain. This is not necessarily due to direct contact with the head. Several common features that incorporate clinical, pathologic, and biomechanical injury constructs that may be utilised in defining the nature of a concussive head injury include the following: Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an “impulsive” force transmitted to the head. Concussion typically results in the rapid onset of short-lived impairment of neurologic function that resolves spontaneously. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course; however, it is important to note that in a small percentage of cases, post-concussive symptoms may be prolonged. No abnormality in standard structural neuroimaging studies is seen in concussion. Symptoms: The symptoms of concussion can vary from case to case, and can be numerous in nature. Symptoms that may arise can include: Headaches Fogginess Loss of consciousness Balance impairment Irritable behaviour Slowed reaction times Sleep/wake disturbance Dizziness Difficulty concentrating Word-finding problems Depression Impulsiveness Nausea and vomiting Only one of these symptoms is required following a head injury to diagnose an individual with a concussion. Symptoms often last for 7-10 days following the incident, however can last for several months in severe circumstances, in these cases the patient is then diagnosed with “post-concussion syndrome”. Concussion Prevention There is no good clinical evidence currently available that shows protective equipment will prevent concussion. Biomechanical studies have shown a reduction in impact forces to the brain with the use of head gear and helmets, but these findings have not been translated to show a reduction in concussion incidence in randomised control trials. Instead helmets are proven to be effective at preventing other forms of head trauma such as skull fracture as a result of a fall. A major concern with the recommendation of helmet use in sport is “risk compensation”, whereby athletes take on more reckless behaviour with the misguided belief that the protective equipment will stop all injury, resulting in the adoption of more dangerous playing techniques. This is particularly a concern in children’s sports where head injury rates are often higher than in adults (Hagel & Meeuwisse, 2004). In a study performed by Hrysomallis in 2016, it was found that isometric neck strength was directly related to an individuals’ injury risk. This study also found that athletes with a history of concussion had decreased values for isometric neck strength in pre-season compared to athletes with no history of concussion. It has been demonstrated that greater isometric neck strength reduced the kinematic response of the head upon impact in male and female athletes who play contact sports. Collins et al performed a study in 2014 which ascertained that a one pound increase of neck strength was associated with a 5% decrease in the risk of concussion. Graduated Return to Play Protocol following Concussion: Rehabilitation Stage Functional exercise at each stage of rehabilitation Objective at each stage No activity. Complete physical and cognitive rest. Recovery. Light aerobic exercise. Walking, swimming, or stationary cycling at approximately 50% intensity. No resistance training. Increase heart rate. Sport-specific exercise. Running drills. Add movement. Non-contact training drills. Passing drills. Exercise, coordination and cognitive load. Full contact practice. Normal training activities. Restore confidence and assess functional skills. Return to play. Normal game play It is recommended that a player remains asymptomatic for 24 hours at stage 1 before progressing to stage 2 of rehabilitation. If any symptoms resurface during the progression of stages, athletes should revert back to the previous stage for a further 24 hours before attempting to re-progress. Risk of Premature Return to Play: Risk of further injury: The principal concern of premature return to play of a concussed athlete is that, because of impaired cognitive function the athlete will sustain further injury (either concussive or other musculoskeletal injury) when returning to a dangerous playing environment. Second Impact Syndrome (SIS): A term used to describe the potential catastrophic consequences resulting from a second concussive blow to the head before an individual has fully recovered from the symptoms of a previous concussion. This is believed to result in loss of cerebrovascular auto-regulation, which in turn leads to brain swelling secondary to increased cerebral blood flow. Concussive convulsions: A variety of immediate motor phenomena or convulsive movements may accompany a concussion. Although dramatic, these clinical features are generally benign and require no specific management beyond the standard treatment of the underlying concussive injury. This phenomenon is a non-epileptic manifestation of concussion. Prolongation of symptoms: If a player recommences playing while symptomatic, post-concussive symptoms may be prolonged. This may also increase the chance of developing “post-concussive syndrome,” in which fatigue, difficulty in concentration, and headaches persist for some time, often months, following the original injury. Exercise appears to prolong the condition. Chronic Traumatic Encephalopathy (CTE): A risk of recurrent concussions during contact sporting careers. Athletes who are subjected to recurrent concussions, disproportionately suffer from mild cognitive impairment, and other mental health problems. Research is demonstrating that a small percentage of these athletes seem to suffer from chronic or long-term sequelae
- All Posts
- Acupuncture
- Dietetics
- Ergonomics
- Infertility
- Nutrition
- Physiotherapy
- Pilates
- Podiatry
- Pregnancy
- Remedial Massage
- Sports Injuries
- Stretches
- Workplace Physiotherapy

Is it a Corn or Callus? Are you a dusk-until-dawn party goer? Or maybe you work long hours standing up?...

We have all heard it before about how growing old sucks and the body breaks down. If I had a...

With the weather warming up we can all begin to think about dusting off our swimmers and taking a dip...

5 Chronic Pain Myths Chronic pain, or pain that sticks around for longer than three months, affects one in five...

Must we sit? Have you ever considered how much sitting you do on a daily basis? How much of this...

Adequate and appropriate recovery is essential for allowing the body to adapt to training loads, repair its self and prevent...

Do we look after our hands enough? Firstly, if we take a look at the wrist, it contains many small...

With 24/7 gyms popping up all over the place, the health department increasing their emphasis on exercise promotion, everyone trying...
Categories
Recent Posts
-
 Forefoot vs rearfoot striking14 Jan 2022
Forefoot vs rearfoot striking14 Jan 2022 -
 Flexibility - To Stretch or Foam Roll?07 Jan 2022
Flexibility - To Stretch or Foam Roll?07 Jan 2022 -
 Creams, Gels & Lotions16 Sep 2021
Creams, Gels & Lotions16 Sep 2021 -
 Hamstring Strains13 Aug 2021
Hamstring Strains13 Aug 2021 -
 Motor Vehicle Accidents (MVA) and Physiotherapy02 Aug 2021
Motor Vehicle Accidents (MVA) and Physiotherapy02 Aug 2021 -
 Relative Energy Deficiency in Sports syndrome (RED-S) and stress fractures13 Jul 2021
Relative Energy Deficiency in Sports syndrome (RED-S) and stress fractures13 Jul 2021 -
 Patellofemoral Pain Syndrome (PFPS)02 Jul 2021
Patellofemoral Pain Syndrome (PFPS)02 Jul 2021 -
 Concussion25 May 2021
Concussion25 May 2021 -
 Thoracic Outlet Syndrome14 May 2021
Thoracic Outlet Syndrome14 May 2021 -
 Lower back pain - the basics07 May 2021
Lower back pain - the basics07 May 2021